It’s been a tough year for Humana (No. 39 on the Fortune 500), the health-insurance giant that primarily serves seniors enrolled in Medicare Advantage plans. Rising medical costs and a drop in the quality ratings that are used to calculate bonus payments have made an impact. On Nov. 5, Humana reported a drop in net income to $1.62 a share, from $3.98 a share the year prior, and lowered its full-year earnings guidance.
CEO Jim Rechtin, who has been in the role since July 2024, spoke to Fortune prior to the release of earnings, and discussed how he’s navigating a tough climate and trying to transform Humana.
This interview has been edited and condensed for clarity.
You started your career in the Peace Corps, directing a public health and water sanitation project in what’s today the Republic of Congo. What did you learn from that experience?
Six months in, I was ready to quit and go home. We were doing construction projects to build latrines and cap wells and we expected the communities to fund those things themselves.
They’re sitting there, saying ‘I have a stream in my backyard that has perfectly clear water in it.’ As we began to ask questions, people would come back to say, ‘Well, we need latrines in the market. We need latrines at the school, the hospital.’ So we were able to target the project in a different way. The fundamental lesson is, go talk to your customers and ask them what they need, because they know.
You’re assigned this project, but the project doesn’t work because nobody’s been on the ground there and you spend your first year realizing it’s not going to work. So you start talking to people and listening to them and you realize that we misunderstood the need. That really is, frankly, no different than my first year and a half here.
Humana is like the Peace Corps?
You come in with an idea of what needs to happen, but the reality is you don’t know.
So you spend a whole bunch of time going out, talking to members, providers, your own associates, and you begin putting ideas together.
Most of my background has been in the provider space, not the insurance space. We’re both, but we’re predominantly in the insurance space. The challenge there is that it’s a business built around managing a high volume of transactions and pricing risk, but it’s not a business that is inherently attuned to consumers. If you interviewed a bunch of our 65,000 associates, you’d walk away and say, ‘Hey, these are good people. They really care about customers.’ Then you would realize that we have almost no tools to collect feedback from our customers.
A lot of what we’re trying to do now is behave more like a consumer health care company, to the degree that there is such a thing in the U.S. right now, as opposed to a traditional insurance company. That starts with understanding who your customer is and getting feedback and trying to balance that multiyear journey with the near-term pressures.
Once you get all that feedback, are there some inherent constrictions with the business model in terms of incorporating it?
I don’t want to pretend that there aren’t obstacles, but I would say that they’re not structural to the business or the sector. They are obstacles of history, the cultural biases that we bring to every conversation. It’s the way that we have chosen to do things that we have to unwind.
Any examples?
We recently rolled out a new portal for the annual enrollment process. What we have never done before is say: Let’s rapidly prototype one in 30 days, trial it with a bunch of real consumers, get feedback, modify the next 30 days, get feedback again and so on. We would have typically come up with a six-month plan to build something, with no input from the people who are going to use it and then find out that we didn’t build it quite right. There’s no structural reason to do it one way or another.
Your customer base must skew older because the bulk of your revenue comes from Medicare Advantage (private Medicare-approved plans that often offer extra benefits like vision, dental and fitness coverage).
Yes, most of our business is built to serve seniors. We do have other businesses that don’t serve seniors, and those are growing, but we predominantly serve seniors. They’re on Facebook, they use YouTube, they shop on Amazon. They may not be as digitally native as a 25-year-old, but they’re absolutely digitally engaged. Sometimes we get caught up in the bias that they’re not. We need to give them the type of experience that they want to engage with. We sponsor the Senior Games, kind of like the Olympics for seniors, and this year we rolled out an adjacent event called the Cognitive Games.
Cognitive games?
It’s things like Bejeweled and Wordle and those kinds of games. In the first week, we engaged a few hundred thousand people, so we knew we’d built something that they wanted.
How does that help the Humana band?
On the Cognitive Games, I don’t know the answer. For what it’s worth, we didn’t start sponsoring the Senior Games because we were looking for an ROI. We thought it was a good thing to do, as a civic contribution. We almost stumbled into the ROI by accident because we were seeing people enrolling at the Senior Games or after.
The bigger thing is how it changed perceptions of our brand. If you were to interview people at the Senior Games about Humana, they would tell you that it’s about wellness, taking an interest in the whole person’s health. That goes beyond a let-me-pay-your-claim consumer health care company. We’re out where consumers are, building a relationship with them. We’re not managing a payment transaction in the shadows.
Any thoughts on the current administration’s moves to cut health care costs?
Health care is one of the largest expenditures in the federal and state budgets. There’s not much that goes on in the policy world that doesn’t have some second- or third-order implication for us. So, yes, we pay attention. Yes, it matters. I think we should all be concerned about the fiscal pressures that the country is under right now. Those fiscal pressures and the size of health care expenses means there will continue to be pressure on our sector.
There are these opposing forces: One is the fiscal realities of our country and our government; the other is an active voter block that really loves Medicare and Medicare Advantage. Those two things are pushing on each other, and we sit in between. We can play that role passively and hope that those two pressures resolve themselves, or we have an opportunity to be proactive in trying to diffuse that pressure, taking a more active stance in helping consumers make good health care decisions, which will reduce costs over time. Most consumers want to make good health care decisions. They need information and the tools to be able to do that. And so we can play a more active role. To me, that goes right back to being a consumer health care company.
“Most consumers want to make good health care decisions. They need information and the tools to be able to do that.”
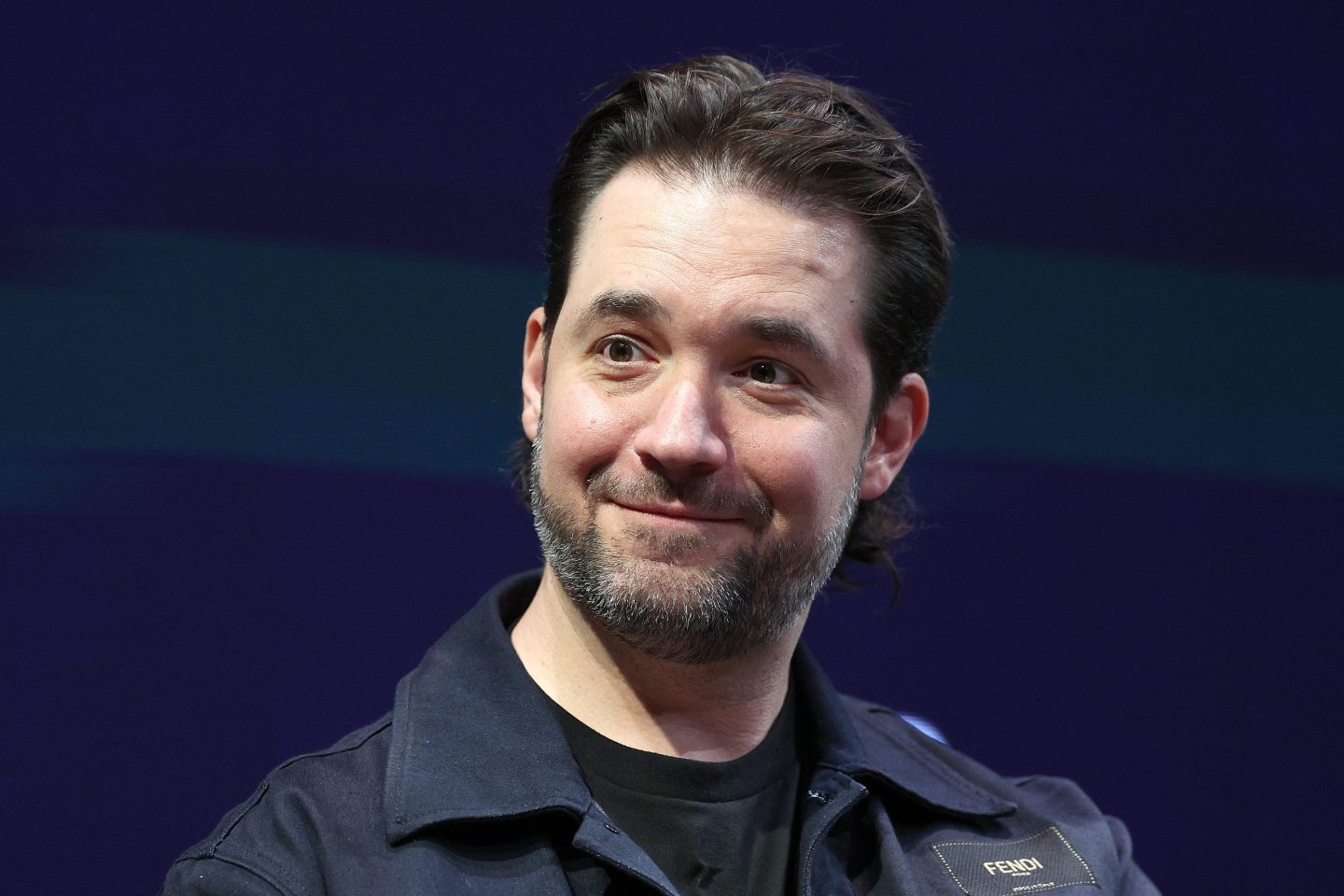
Jim Rechtin, CEO, Humana
What are we not paying enough attention to, in terms of the opportunities or the challenges?
Most of the conversation is about one annual budget after another. The things that we need to fix are not going to be fixed in an annual budget cycle. How do we get a more holistic solution to the fiscal pressures and the health care components?
What would you do?
How do you take the unnecessary utilization out of the system? And how do we streamline and simplify the system in a way that takes a whole bunch of the bureaucratic cost out of it? That’s not limited to any one sector. A lot of that has to do with how the different sectors of health care interact with each other. Billing and collecting costs too much. Distribution costs too much. The hurdles to access create unnecessary cost. We need more modern pipes to exchange data between the different players in the industry. We need, frankly, more access to data so that we can better inform and guide and educate our members on how to access care. The fragmented nature of how our system works creates friction. It creates cost. And a lot of that is about not being modernized.
Is AI as transformative as we make it out to be in this space?
It will be over the next five years. You can’t move as fast as you’d like to roll out the capability, the tools. But yes, health care and the industry and the economy more broadly are going to look very different.
How are you using it right now?
Let me give you examples. We are rolling out ambient listening technology that takes the administrative burden of being a doctor off our doctors and allows them to spend more time with the patient. We have a new tool that we just rolled out for our brokers and sales agents that we refer to as Agent Assist that allows them to streamline a very complicated sales process. For Medicare Advantage, they have to comb through dozens and dozens of documents. AI can comb through all of those documents on an automated basis and answer very basic questions much more rapidly, shortening the sales cycle and getting frankly more accurate answers. Eventually, consumers are going to interact with it directly. We can’t do that yet, but that’s coming, probably three years from now.
If we want real-time approvals of requests, then we want AI for prior authorizations. But we want it to say yes, not no, right? Right now, we use AI tools to get to a faster yes. The nos go to a doctor who can get better documentation in front of them faster to make that process more efficient.
What do we do for this next generation of entry-level workers that may not have a lot of job opportunities right now?
I grew up predominantly in Indianapolis and a little bit in Kentucky. That was my whole life. I spent very little time in any other part of the country. During my sophomore year, I did a service trip to Appalachia. I spent a month mostly living with a family there, and I walked away realizing how different life is only a couple hundred miles away from where I grew up. It got me curious: What’s it like elsewhere? So I did a service trip to Honduras and then the Dominican Republic. I wanted to learn more. And that’s what led me to the Peace Corps.
What I wanted to do is live in a community that was very different from the community I grew up in. Experiencing new things is really what’s valuable from a learning experience. If we are going to find ourselves in a world where entry-level jobs are harder to come by, and the economy is in transition, and we need to find mechanisms to allow a generation of kids to keep growing, to get those new experiences.
What did it teach you about yourself?
I was a political science major. We talked about rule of law and democracy. You don’t really understand what those are until you’re in a place where they aren’t. That was probably the biggest thing that was eye-opening for me, to be in a place where you don’t have a mature judicial system or legal system. But the biggest thing that I realized is the power of asking questions.
Five years from now, will Humana look different?
It better, because if it doesn’t look different, it won’t survive, right? I think that’s true of everybody. Humana has unique positioning to have a real impact on how improved quality care reduces total cost. We serve seniors, who have a lot of health care needs, and it’s an individual product so you can tailor the product. Third, we are also in the primary care space. We’re in the home health space. We have our own ability to distribute medication in areas that have the greatest ability to impact chronic conditions and the total cost of delivering health care services. I think you can really have an impact on both cost and quality of care.
How do you want people to think about the brand?
If we’re going to stop being viewed as a health insurance company and start being viewed as consumer health care company, we need to engage our members in a way that does two things. One is arm them with what they need to make better health care decisions on the front end to avoid or delay downstream issues. Second, help them navigate the system. We’re not the provider who touches them every day, but we have more data and more knowledge about those providers and about the experience that they are going to have with them than anybody else. We have never stepped back and fully acknowledged that we have agency in that experience.
So you’ve been more of a passive actor in the background in that process?
Way too often. That’s what health insurance has been: They’ve been passive actors.
So what are your priorities right now?
We are not where we want to be, and we’ve been very public. The challenge is that when we realized we had fallen behind, we only had three months to fix it. We feel very good about the trajectory that we’re on for next year. We have to get our star ratings right, which means we need to make sure that we are delivering for our customers, both from an experience standpoint and clinical standpoint. That’s number one.
The second priority for us is what I would describe as tech enablement. How do we use technology to better engage members and run more efficiently? Third, how do we really differentiate the experience we are delivering, which is not all technology driven. We’ve simplified our product. We’ve made it easier to access preventative care and we’re taking away the financial hurdles. To do that, we are streamlining the prior authorization process to make it less cumbersome, both for providers and consumers. We are partnering with companies like EPIC (an electronic health record system) to create more cost transparency for our members. At the end of the day, it’s about building an experience that a consumer wants to be a part of.